CASE OVERVIEW
A 23-year-old male with a history of horizontal nystagmus and contact lens intolerance was interested in vision correction surgery. Refractive error in the right eye was -3.50 -1.75 x 65, which allowed 20/30 acuity, and in the left eye, -4.75 -2.00 x 170, which allowed 20/40 acuity.
Corneal thickness measurements were 540 microns in the right eye and 557 microns in the left eye. Computerized topography showed no evidence of irregular astigmatism. Anterior segment examination was normal except for the finding of the horizontal nystagmus.

WHAT ARE THE TREATMENT OPTIONS TO CORRECT HIS MYOPIA AND ASTIGMATISM ? DOES THE NYSTAGMUS INTERFERE WITH AN IDEAL OUTCOME?
Both LASIK and PRK are reasonable options to obtain best uncorrected acuity. Given the finding of horizontal nystagmus, it was felt that PRK would be a safer option to decrease the potential of flap slippage and the need for surgical repositioning.
WHAT WAS DONE:
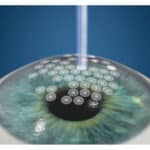
PRK was performed in both eyes, and a rotary brush was used to remove 9 mm of central epithelial cells in both eyes. The high speed active eye tracker was used at the time of the excimer ablation treatment. Mitomycin C was applied for 30 seconds to decrease the risk of corneal haze.
Postoperatively, the eyes healed well, and the bandage contact lenses were removed at 5 days. Uncorrected acuity continued to improve, and at 3 weeks postop, he had an uncorrected acuity of 20/40 in the right eye and 20/50 in the left. This gradually improved over time, achieving an uncorrected acuity which was similar to the preop best corrected acuity.