
CASE SUMMARY
A 25-year-old male presented for a refractive surgery evaluation with a refractive error of +5.25 -3.50 × 155 in the right eye (20/25 vision) and +6.00 -4.50 × 12 in the left eye (20/25 vision). Corneal topography revealed high regular corneal astigmatism.
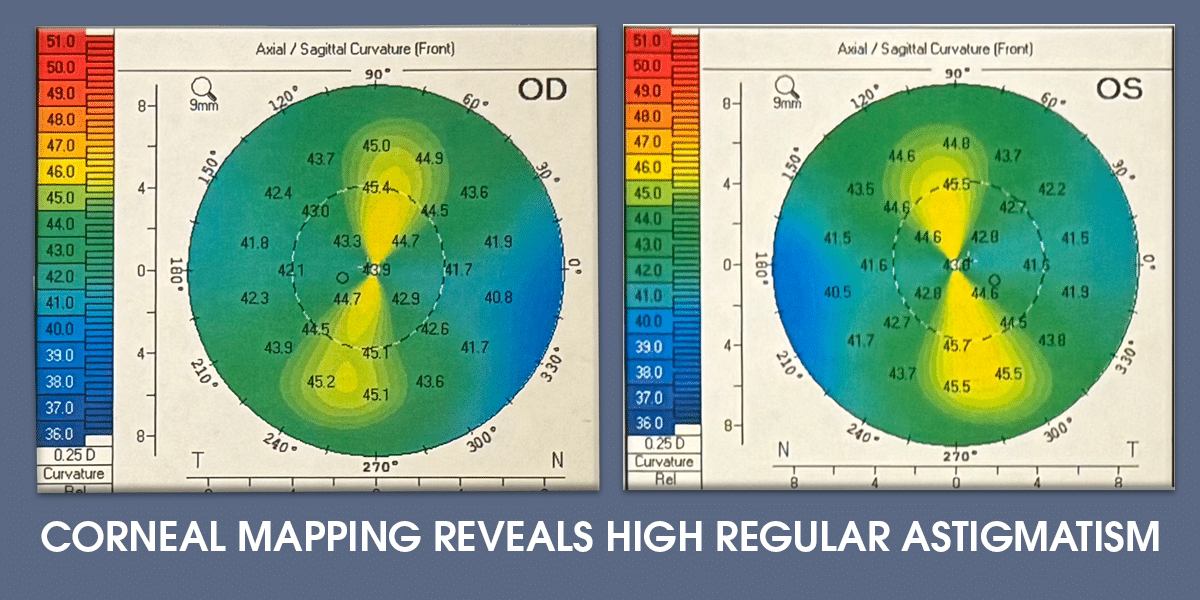
REFRACTIVE SURGERY CONSULTATION
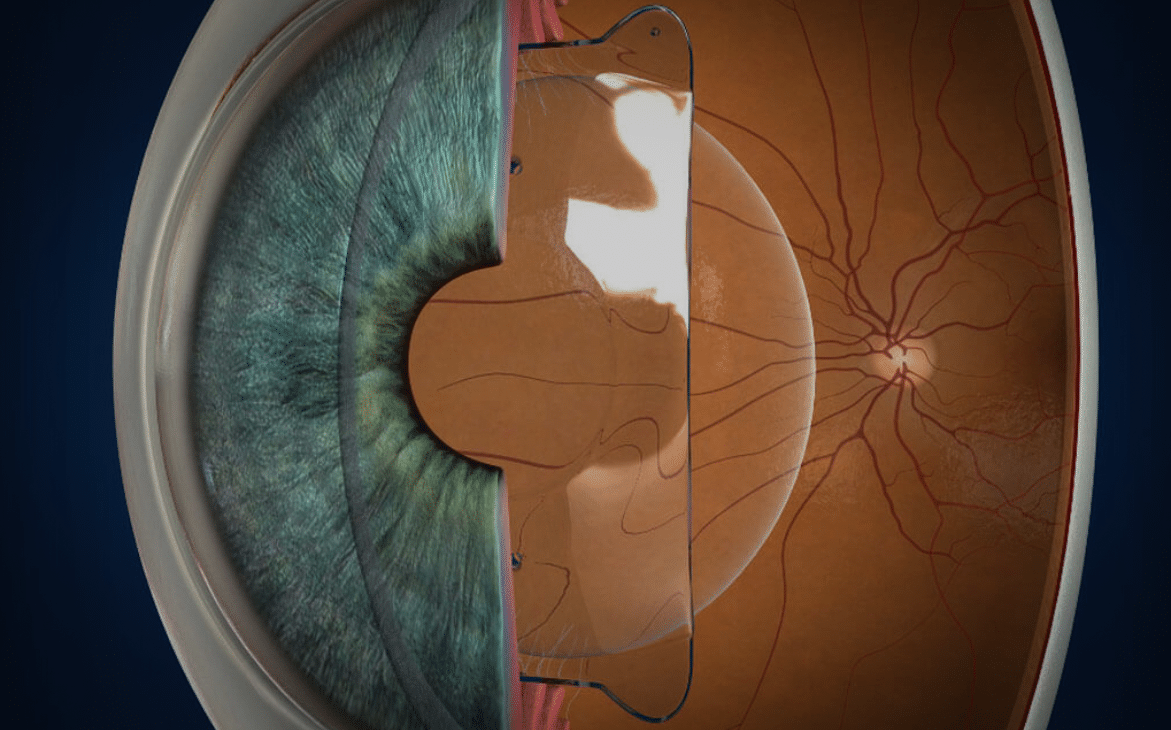
Various refractive surgery options were discussed. Laser vision correction was deemed unsuitable due to the high refractive error, which would steepen the cornea excessively, increasing the risk of regression and dry eye. His anterior chamber depth measured 3.68 mm in the right eye and 3.58 mm in the left, qualifying him for hyperopic Implantable Contact Lens (ICL) surgery.
The risks and benefits of ICL placement were reviewed, and the patient opted for the procedure. Preoperative peripheral iridotomies were performed at 10 and 1 o’clock in both eyes to prevent pupillary block glaucoma, as hyperopic ICLs lack a central port.
INITIAL POSTOPERATIVE COMPLICATIONS
At the one-day follow-up, the patient’s uncorrected vision was 20/400 in each eye. Examination revealed a 40-degree rotation of the ICLs, significantly increasing astigmatism. Importantly, the ICLs did not obstruct the superior iridotomy sites, avoiding elevated intraocular pressure. The vault, distance between the ICL and crystalline lens was 100 microns. The recommended vault from Staar, the manufacturer of the ICL, is 250 to 750 microns with an average of 475 microns.
FINAL OUTCOME
Both original ICLs were removed and to address the lens rotation, new lenses were custom ordered with a larger diameter. The new ICLs had a diameter of 13.2 mm compared to the previous size of 12.1 mm. If the rotation of the ICLs was less than 15 degrees, then we would have opted for simple repositioning.
One day after the final procedure, the patient’s uncorrected vision improved to 20/25+ in both eyes, with stability confirmed at one month. The patient expressed satisfaction with the outcome.
KEY LEARNING POINTS:
This case highlights the importance of accurate lens sizing and careful preoperative planning to ensure optimal outcomes for hyperopic and toric ICL procedures.
1. CUSTOM ICL DESIGN & SIZING:
ICLs are custom-manufactured to correct specific refractive errors and fit the individual’s anatomy with a certain diameter.
Lens diameter is calculated using white-to-white measurements (e.g., from optical biometers like the Lenstar or Pentacam) or sulcus-to-sulcus measurements via B-scan ultrasound.
2. ROTATION & ASTIGMATISM:
Lens rotation can result in significant astigmatism if the ICL diameter is too small. In this case, a larger lens provided stability and proper alignment, correcting the astigmatism.
3. HYPEROPIC ICLs & IRODOTOMY:
Unlike myopic ICLs with a central port, hyperopic ICLs necessitate preoperative iridotomies to prevent pupillary block glaucoma.
4. ANTERIOR CHAMBER DEPTH REQUIREMENTS:
Hyperopic ICLs require a minimum anterior chamber depth of 3.0 mm, measured from the corneal endothelium to the anterior crystalline lens. This depth exceeds the 2.8 mm minimum for myopic ICLs.


