CASE OVERVIEW
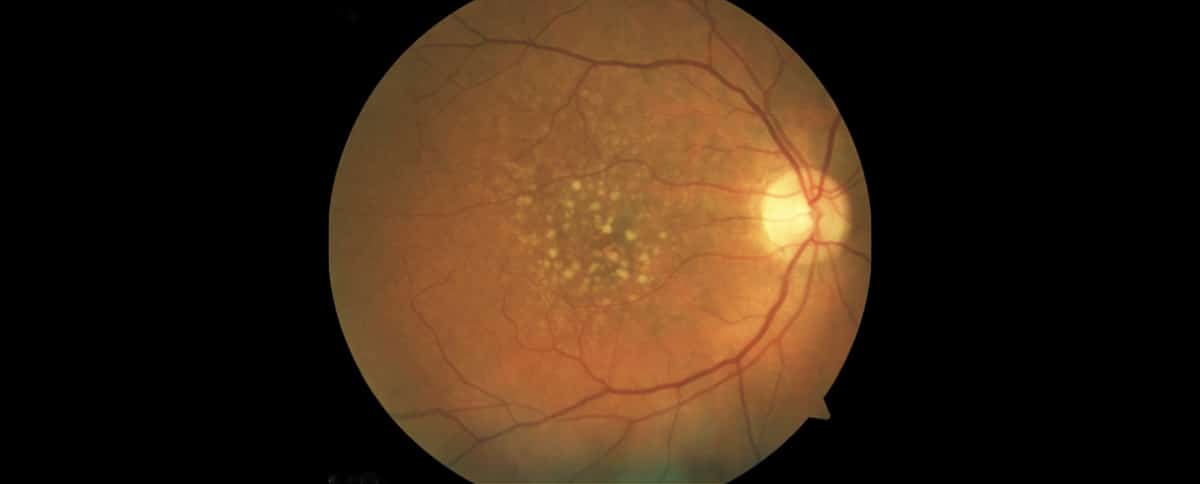
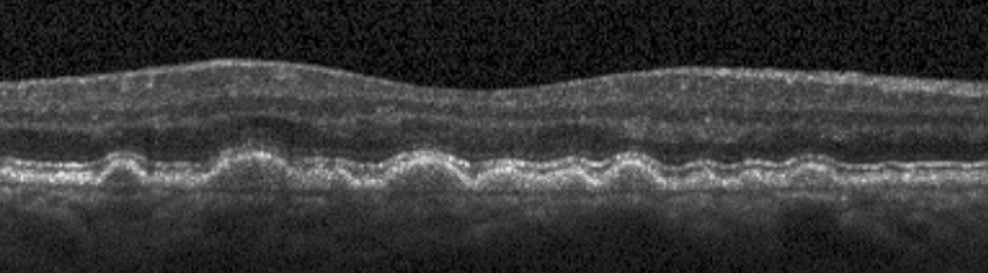
A 76-year-old woman presented with gradually decreasing vision in both eyes. On examination, her best-corrected visual acuity was 20/100 in the right eye and 20/80 in the left. She was found to have 2-3+ nuclear sclerosis and 2+ nuclear cortical cataracts in both eyes. Fundus examination and OCT of the macula revealed age-related macular degeneration (AMD) with the presence of macular drusen.
SURGICAL OPTIONS:
A potential acuity test can help assess macular function. In this case, the right macula had the potential to achieve 20/40 vision, while the left had the potential for 20/50 vision.
WHAT WAS DONE:
Based on this information, selecting the most appropriate intraocular lens (IOL) is crucial. Given the presence of AMD, a multifocal IOL is contraindicated. Instead, either an extended-depth-of-focus or an advanced monofocal IOL could be used, depending on the desired vision outcome (distance, mini-mono vision, or near vision). Since the patient does not drive and spends most of her time reading or engaging in indoor activities, an advanced monofocal IOL (Eyhance) was selected to create a mini-mono effect.
The result was plano in the right eye with 20/40 vision and -1.25 in the left eye with J4 near vision. The patient was satisfied with the outcome.
KEY LEARNING POINTS:
- Preoperative OCT testing of the macula is crucial to rule out subtle macular pathology, particularly when cataract severity impedes fundus visualization.
- OCT findings guide IOL selection, as multifocal implants are contraindicated in the presence of AMD.
- Detecting macular abnormalities preoperatively helps manage patient expectations regarding postoperative vision outcomes.


