
CASE OVERVIEW
A 28-year-old male was referred with unilateral keratoconus. He underwent corneal crosslinking (CXL) in his keratoconus eye and was then followed on an annual basis to determine success of the CXL and any changes to his “normal” eye. Two years postoperatively, his keratoconus eye showed stability, and his uncorrected visual acuity in the other eye remained at 20/20.
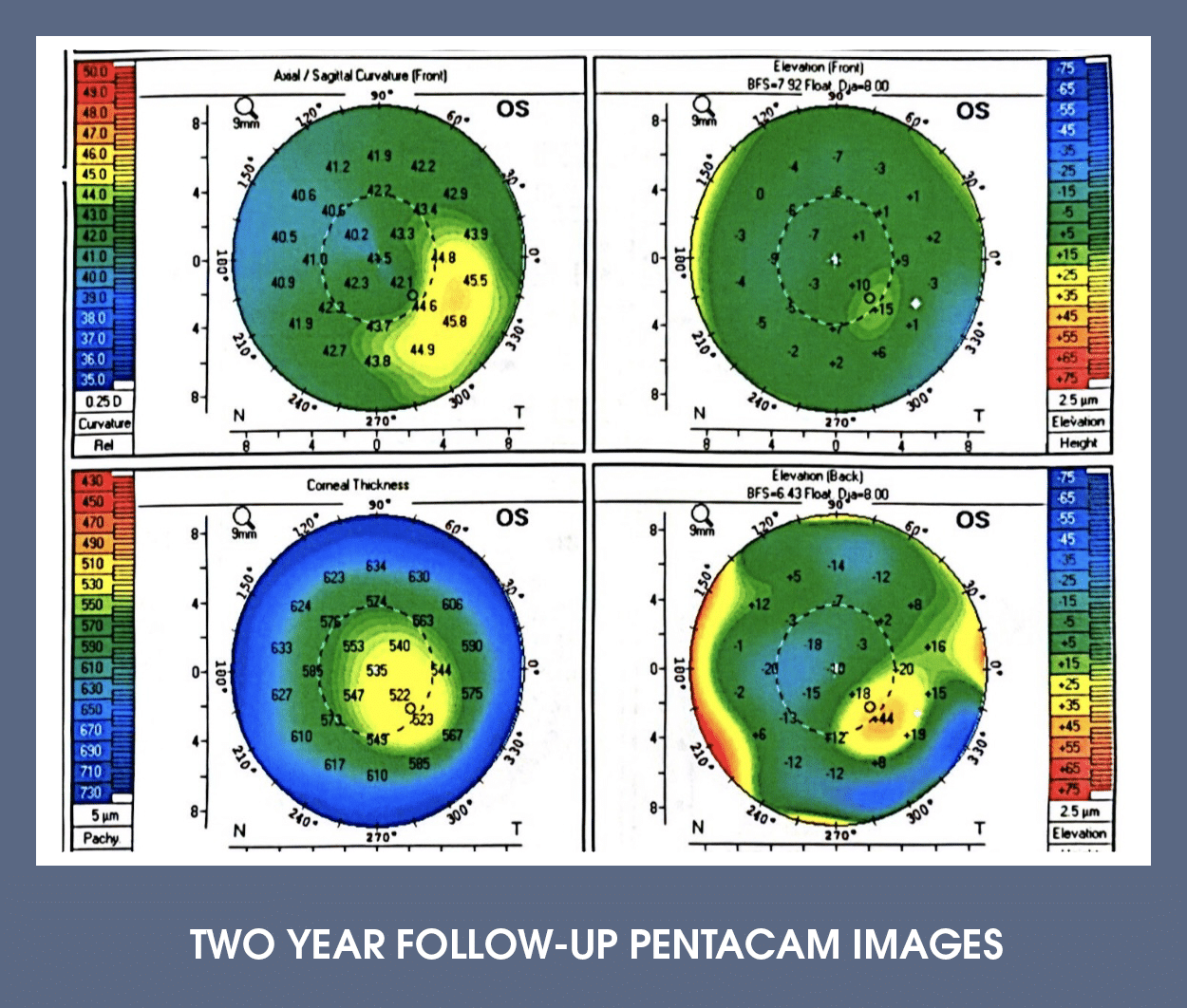
However, computerized tomography revealed early signs of keratoconus in the left eye. The Pentacam maps below showed infero-temporal steepening, thinning located in the steep part of the cornea, and posterior elevation. His refractive error in this eye was plano-0.50 x 130.
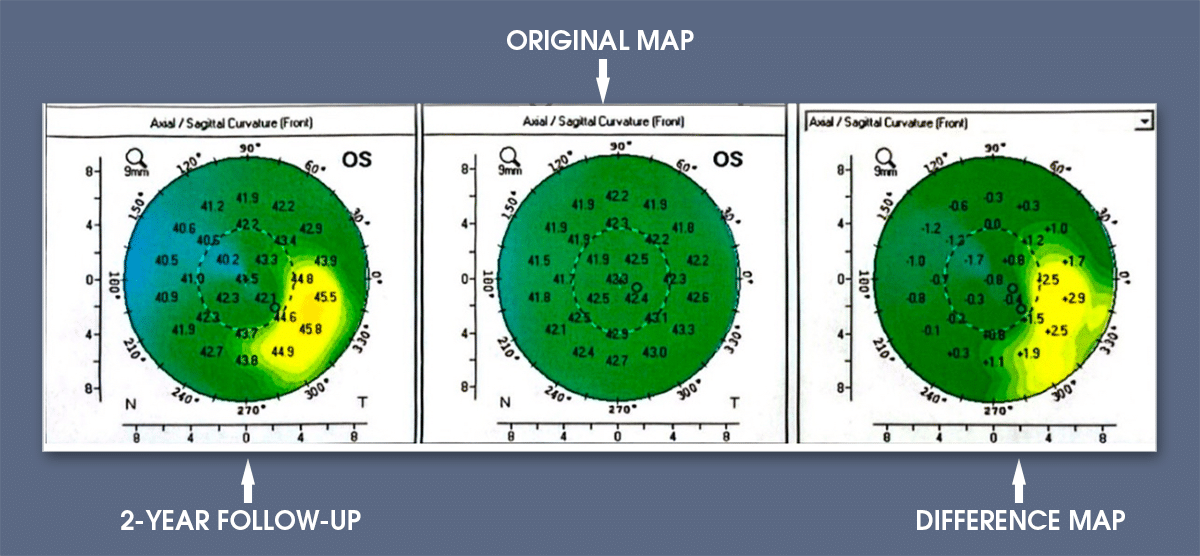
The difference maps from computerized tomography indicated a significant progression in the left eye over the past year, with 2.9 diopters of steepening infero-temporally. Essentially the eye went from ‘normal’ to keratoconus. As a result, the patient underwent CXL in this eye.
KEY LEARNING POINTS:
1. EARLY KERATOCONUS MAY NOT AFFECT VISUAL ACUITY: Patients can exhibit keratoconus with an excellent uncorrected acuity, as peripheral corneal changes (anterior and/or posterior, thinning) may occur without impacting central vision or refractive error.
2. CORNEAL TOMOGRAPHY IS IMPORTANT FOR MONITORING PROGRESSION: Follow-up should include corneal tomography, which assesses both the anterior and posterior cornea as well as corneal thickness. Early changes often occur in the posterior cornea, which could be missed with anterior curvature evaluation alone.
3. REFRACTIVE ERROR CHANGE IS A LATE SIGN OF PROGRESSION: Changes in refractive error are typically a late manifestation of keratoconus and indicate substantial corneal distortion.
4. CORNEAL CROSSLINKING IS THE STANDARD TREATMENT FOR PROGRESSION: CXL remains the primary intervention to prevent further progression of keratoconus. If there is a decrease in best-corrected acuity, then combining CXL with TG-PRK increases the likelihood of improving acuity.


