
CASE OVERVIEW
A 37-year-old woman presented to the Bochner Eye Institute with a long-standing decrease in vision in her right eye following LASIK performed in China two years earlier. Having recently emigrated to Canada, she sought correction to improve her visual acuity.
EXAMINATION FINDINGS:
- Uncorrected Visual Acuity (UCVA):
- Right eye: 20/60
- Left eye: 20/25
- Best-Corrected Visual Acuity (BCVA):
- Right eye: 20/40 with -1.00-1.50×90
- Corneal Findings:
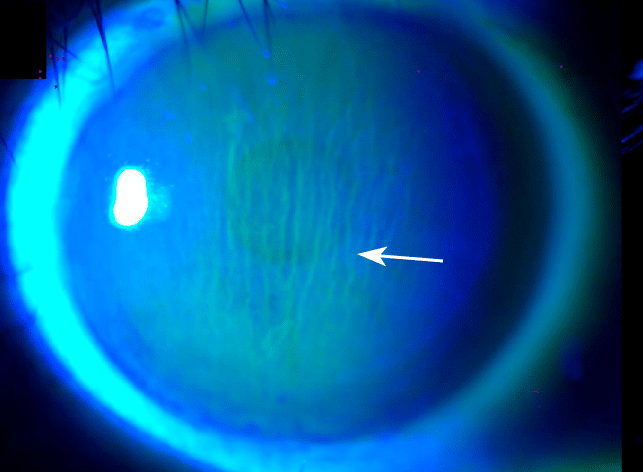
- Right eye: Significant vertical macrostriae extending through the pupil.
- Left eye: Clear flap without evidence of striae.
- Corneal Topography:
- Right eye: Moderate irregular astigmatism.
- Left eye: Smooth cornea with central flattening.
DIAGNOSIS & TREATMENT:
The patient was diagnosed with long-term macrostriae in the right eye, identified as the primary cause of her decreased vision. Surgical repair was recommended.
The procedure involved lifting the LASIK flap, stretching it to smooth the corneal surface, and securing the flap with multiple sutures. At one month postoperatively, the sutures were removed, and the cornea appeared clear. By the five-week follow-up, the patient achieved an uncorrected visual acuity of 20/25 in the right eye and reported significant satisfaction with her improved vision.
KEY LEARNING POINTS:
1. CHRONIC MACROSTRIAE:
- Rare and often indicative of mild flap subluxation.
- Treatment requires aggressive stretching and often the placement of sutures.
- Removal of epithelium on the bed near the flap margin is necessary to minimize the risk of epithelial ingrowth.
2. EARLY MANAGEMENT OF MICROSTRIAE:
- Microstriae detected shortly after LASIK can be corrected by lifting the flap, stretching it in the opposite direction, and repositioning it.
- If identified within 24 hours of surgery, flap smoothing can often be performed at the slit lamp.
- Prognosis is excellent with prompt intervention.
3. IMPACT ON VISUAL ACUITY:
- Striae over the pupil typically interfere with visual acuity and may cause glare or halos; these should be repaired.
- Mild peripheral or central striae may not require treatment if the patient is asymptomatic and has good vision.
4. RISK FACTORS FOR FLAP STRIAE:
- IHigher myopic corrections increase the risk due to greater surface area discrepancies between the flap and bed.
- Contributing factors include eye rubbing, excessive blinking, and improper surgical techniques (e.g., misalignment or over-irrigation).
5. DETECTION:
- Most striae are visible at the slit lamp, but subtle cases are best identified using fluorescein dye with cobalt blue light.
- Uneven fluorescein pooling after blinking can reveal their location.
6. POST-OPERATIVE EXAMINATION:
- Early detection is crucial. Patients should be examined 15–30 minutes post-LASIK to confirm flap alignment.
- Uneven gutter width at the flap edge is a key indicator of misalignment.
CONCLUSION:
This case emphasizes the importance of recognizing and managing chronic macrostriae to restore visual quality. Timely surgical intervention can result in significant improvement, even in long-standing cases.


